Open Muscle-Preserving Pedicle Screws Fixation Versus Conventional Open Posterior Approach in Thoracolumbar Burst Fracture without Neurologic Injury
DOI:
https://doi.org/10.56929/jseaortho.v46i1.20Keywords:
burst fracture, spine surgery, minimally invasive surgery, pedicle screwAbstract
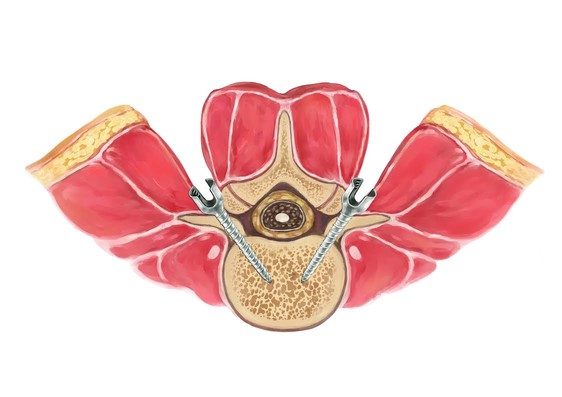
Introduction: Patients who sustained thoracolumbar spine fracture without neurological deficit often require surgical treatment. The conventional open posterior approach had some disadvantages including post-operative pain, blood loss, and duration of the operation. The minimally invasive approach, open muscle-preserving pedicle screw fixation, was proposed to have more benefit than the conventional approach. This study evaluated the clinical and perioperative outcomes of thoracolumbar burst fracture fixation using the open muscle-preserving approach and the conventional open posterior approach.
Methods: A prospective cohort study from June 2016 to June 2017 of the open muscle-preserving pedicle screw fixation approach was done compared to the historical control of the conventional open posterior approach from May 2015 to May 2016. The post-operative pain score, blood loss, duration of operation and clinical outcome were analyzed.
Results: Twenty-three patients were enrolled in the muscle-preserving approach group, and 27 patients treated with the conventional open posterior approach were the control group. Post-operative VAS was significantly better in the muscle-preserving group (P<0.001). The mean operating time was significantly shorter in the muscle-preserving group (60.4±17.3 min. vs. 90.9±18.9 min., p<0.001). Moreover, the mean intra-operative blood loss of the muscle-preserving group was also significantly lower (156.96±96.3ml. vs. 269.26±147.6ml., p=0.003).
Conclusion: Our study results indicate a superiority of the open muscle-preserving approach over the conventional open posterior approach for a thoracolumbar burst fracture without neurologic injury in terms of post-operative pain score, blood loss and duration of operation. The open muscle-preserving approach is an alternative treatment for thoracolumbar burst fractures.
Metrics
References
Foley KT, Gupta SK, Justis JR, et al. Percutaneous pedicle screw fixation of the lumbar spine. Neurosurg Focus 2001;10:E10.
Holmes JF, Miller PQ, Panacek EA, et al. Epidemiology of thoracolumbar spine injury in blunt trauma. Acad Emerg Med 2001;8:866-72.
Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976) 1992;17:528-40.
Diaz JJ, Jr., Cullinane DC, Altman DT, et al. Practice management guidelines for the screening of thoracolumbar spine fracture. J Trauma 2007;63:709-18.
Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8:817-31.
Cahueque M, Cobar A, Zuniga C, et al. Management of burst fractures in the thoracolumbar spine. J Orthop 2016;13:278-81.
Kawaguchi Y, Yabuki S, Styf J, et al. Back muscle injury after posterior lumbar spine surgery. Topographic evaluation of intramuscular pressure and blood flow in the porcine back muscle during surgery. Spine (Phila Pa 1976) 1996;21:2683-8.
Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. A histologic and enzymatic analysis. Spine (Phila Pa 1976) 1996;21:941-4.
Sihvonen T, Herno A, Paljarvi L, et al. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine (Phila Pa 1976) 1993;18: 575-81.
Cox JB, Yang M, Jacob RP, et al. Temporary percutaneous pedicle screw fixation for treatment of thoracolumbar injuries in young adults. J Neurol Surg A Cent Eur Neurosurg 2013;74:7-11.
Court C, Vincent C. Percutaneous fixation of thoracolumbar fractures: current concepts. Orthop Traumatol Surg Res 2012;98:900-9.
Kim DY, Lee SH, Chung SK, et al. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine (Phila Pa 1976) 2005;30:123-9.
Garfin SR, Fardon DF. Emerging technologies in spine surgery. Spine J 2002;2:1-4.
Rampersaud YR, Foley KT, Shen AC, et al. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976) 2000;25:2637-45.
Wiltse LL, Bateman JG, Hutchinson RH, et al. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 1968;50:919-26.
Ota M, Neo M, Fujibayashi S, et al. Advantages of the paraspinal muscle splitting approach in comparison with conventional midline approach for s1 pedicle screw placement. Spine (Phila Pa 1976) 2010;35:E452-7.
Mehren C, Siepe CJ. Neuroforaminal decompression and intra-/extraforaminal discectomy via a paraspinal muscle-splitting approach. Eur Spine J 2016;25Suppl 2:276-7.
Junhui L, Zhengbao P, Wenbin X, et al. Comparison of pedicle fixation by the Wiltse approach and the conventional posterior open approach for thoracolumbar fractures, using MRI, histological and electrophysiological analyses of the multifidus muscle. Eur Spine J 2017;26:1506-14.
Meng X, Zeng K, Turghunjan A, et al. [Effectiveness of pedicle screw fixation combined with non-fusion technology for treatment of thoracolumbar fracture through Wiltse paraspinal approach]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2014;28:1106-9.
Li H, Yang L, Xie H, et al. Surgical outcomes of mini-open Wiltse approach and conventional open approach in patients with single-segment thoracolumbar fractures without neurologic injury. J Biomed Res 2015;29:76-82.
Kuklo TR, Polly DW, Owens BD, et al. Measurement of thoracic and lumbar fracture kyphosis: evaluation of intraobserver, interobserver, and technique variability. Spine (Phila Pa 1976) 2001;26:61-5; discussion 6.
Phan K, Rao PJ, Mobbs RJ. Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: Systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg 2015;135:85-92.
Korovessis P, Repantis T, Petsinis G, et al. Direct reduction of thoracolumbar burst fractures by means of balloon kyphoplasty with calcium phosphate and stabilization with pedicle-screw instrumentation and fusion. Spine (Phila Pa 1976) 2008;33:E100-8.
Zou DW. [Treatment of unstable fractures of thoracolumbar spine with neurologic injury using a reduction fixation spinal pedicle screws system]. Zhonghua Wai Ke Za Zhi 1992;30:722-5,78.
Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976) 1992;17(8 Suppl):S317-24.
Esses SI, Botsford DJ, Wright T, et al. Operative treatment of spinal fractures with the AO internal fixator. Spine (Phila Pa 1976) 1991;16(3 Suppl):S146-50.
Sasso RC, Cotler HB, Reuben JD. Posterior fixation of thoracic and lumbar spine fractures using DC plates and pedicle screws. Spine (Phila Pa 1976) 1991;16(3 Suppl):S134-9.
Zoidl G, Grifka J, Boluki D, et al. Molecular evidence for local denervation of paraspinal muscles in failed-back surgery/postdiscotomy syndrome. Clin Neuropathol 2003;22:71-7.
Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. Part 2: Histologic and histochemical analyses in humans. Spine (Phila Pa 1976) 1994;19:2598-602.
MacDonald D, Moseley GL, Hodges PW. Why do some patients keep hurting their back? Evidence of ongoing back muscle dysfunction during remission from recurrent back pain. Pain 2009;142:183-8.
Fan Y, Zhang J, He X, et al. A comparison of the mini-open wiltse approach with pedicle screw fixation and the percutaneous pedicle screw fixation for neurologically intact thoracolumbar fractures. Med Sci Monit 2017;23:5515-21.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.