Outcomes of Perilunate Dislocation and Perilunate Fracture Dislocation After a Minimum 1-Year Follow-Up Following Open Reduction and Internal Fixation Via the Dorsal Approach: A Retrospective Study
DOI:
https://doi.org/10.56929/jseaortho-2024-0200Keywords:
perilunate dislocation, perilunate fracture dislocation, modified Mayo wrist score, scapholunate angle, carpal height ratioAbstract
Purpose: This study aimed to review and evaluate the functional and radiographic outcomes of patients with perilunate injuries after a minimum 1-year follow-up following open reduction and internal fixation with or without ligament repair.
Methods: This retrospective study included patients with perilunate injuries who underwent open reduction and internal fixation with or without ligament repair at our hospital between 2013 and 2021 with a minimum 1-year follow-up.
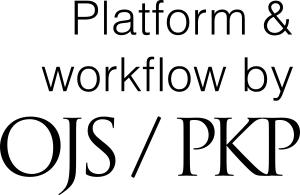
Results: Of the 22 enrolled patients, 18 and 4 exhibited perilunate fracture dislocation and perilunate dislocation, respectively. The mean follow-up period was 15.3 (12–20) months. The mean age of the patients was 30.5 ± 10.2 years. Notably, 20 (90.9%) and 2 (9.1%) patients were males and females, respectively. The mean flexion/extension angles were 67.2°/76.2°. The mean ulnar deviation/radial deviation was 25.4°/13.8°, and the mean pronation/supination was 85.6°/88.3°. As secondary outcomes, the mean grip strength was 80% of the uninjured side, modified Mayo wrist score was 73.6 (1 excellent, 6 good, 11 fair, and 4 poor), and visual analog scale was 0.59. For radiographic outcomes, the mean scapholunate angle (SL angle) was 50.4°, SL gap was 2.43 mm., and carpal height ratio was 0.50. Four and nine patients had an incongruent Gilula's line and arthrosis, respectively.
Conclusions: Satisfactory results can be achieved with open reduction and internal fixation using a dorsal approach. Although some patients had abnormal radiographic findings, the radiographic outcomes may not correlate with the functional outcomes.
Metrics
References
Gracia-Elias M. Carpal instability. Green’s operative hand surgery. 6th ed. Elsevier; 2010. DOI: https://doi.org/10.1016/B978-1-4160-5279-1.00015-0
Kara A, Celik H, Seker A, et al. Surgical treatment of dorsal perilunate fracture-dislocations and prognostic factors. Int J Surg 2015;24:57-63. DOI: https://doi.org/10.1016/j.ijsu.2015.10.037
Gupta RK, Kamboj K. Functional outcome after surgical treatment of perilunate injuries: A series of 12 cases. J Clin Orthop Trauma 2016; 7:7-11. DOI: https://doi.org/10.1016/j.jcot.2015.09.005
Krief E, Appy-Fedida B, Rotari V, et al. Results of perilunate dislocations and perilunate fracture dislocations with a minimum 15-year follow-up. J Hand Surg Am 2015;40:2191-7. DOI: https://doi.org/10.1016/j.jhsa.2015.07.016
Chou YC, Hsu YH, Cheng CY, et al. Percutaneous screw and axial Kirschner wire fixation for acute transscaphoid perilunate fracture dislocation. J Hand Surg Am 2012;37: 715-20. DOI: https://doi.org/10.1016/j.jhsa.2012.01.019
Kremer T, Wendt M, Riedel K, et al. Open reduction for perilunate injuries--clinical outcome and patient satisfaction. J Hand Surg Am 2010;35:1599-606. DOI: https://doi.org/10.1016/j.jhsa.2010.06.021
Forli A, Courvoisier A, Wimsey S, et al. Perilunate dislocations and transscaphoid perilunate fracture-dislocations: a retrospective study with minimum ten-year follow-up. J Hand Surg Am 2010;35:62-8. DOI: https://doi.org/10.1016/j.jhsa.2009.09.003
Budoff JE. Treatment of acute lunate and perilunate dislocations. J Hand Surg Am 2008; 33:1424-32. DOI: https://doi.org/10.1016/j.jhsa.2008.07.016
Souer JS, Rutgers M, Andermahr J, et al. Perilunate fracture-dislocations of the wrist: comparison of temporary screw versus K-wire fixation. J Hand Surg Am 2007;32:318-25. DOI: https://doi.org/10.1016/j.jhsa.2007.01.008
Sotereanos DG, Mitsionis GJ, Giannakopoulos PN, et al. Perilunate dislocation and fracture dislocation: a critical analysis of the volar-dorsal approach. J Hand Surg Am 1997;22:49-56. DOI: https://doi.org/10.1016/S0363-5023(05)80179-0
Hildebrand KA, Ross DC, Patterson SD, et al. Dorsal perilunate dislocations and fracture-dislocations: questionnaire, clinical, and radiographic evaluation. J Hand Surg Am 2000; 25:1069-79. DOI: https://doi.org/10.1053/jhsu.2000.17868
Knoll VD, Allan C, Trumble TE. Trans-scaphoid perilunate fracture dislocations: results of screw fixation of the scaphoid and lunotriquetral repair with a dorsal approach. J Hand Surg Am 2005;30:1145-52. DOI: https://doi.org/10.1016/j.jhsa.2005.07.007
Pinho AB, Sobania RL. Perilunate carpal dislocation. Clinical evaluation of patients operated with reduction and percutaneous fixation without capsular-ligament repair. Rev Bras Ortop 2017;52:402-9. DOI: https://doi.org/10.1016/j.rboe.2017.06.007
Wolfe SW, Kakar S. Carpal instability. Green’s operative hand surgery. 8th ed. Elsevier; 2021.
Abid H, Shimi M, El ibrahimi A, et al. Result of the Sauve-Kapandji procedure for posttraumatic disorder of the distal radioulnar joint in young patients. Open J Orthop 2015;5:35-40 DOI: https://doi.org/10.4236/ojo.2015.53005
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.