Survivorship and Modes of Failure of Varus-Valgus Constrained Implants in Revision Knee Arthroplasty: A Study with a Median Follow-Up of 2.9 Years in an Asian Population
DOI:
https://doi.org/10.56929/jseaortho-2025-0219Keywords:
Varus-valgus constrained, Revision knee arthroplasty, Survival rateAbstract
Purpose: This study aims to evaluate the survival rate, primary causes of failure, and complications associated with varus-valgus-constrained (VVC) implants in revision total knee arthroplasty (TKA) at a large Asian medical institution.
Methods: We retrospectively reviewed 161 patients who underwent revision TKA with VVC implants at our institution between January 2013 and December 2021. Data on patient demographics, initial diagnosis, revision dates, causes of failure, and subsequent re-revisions were collected and analyzed. The Kaplan-Meier method was used to estimate implant survival rates.
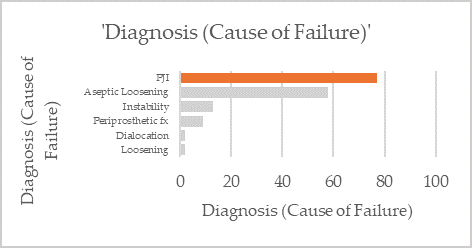
Results: This study included 161 patients who received VVC implant revisions, with a mean age of 73 years at the time of surgery. The mean follow-up period was 2.9 years, extending up to 10.0 years. The primary reasons for revision were infection (47.8%), aseptic loosening (36%), and instability (8.1%). The overall survival rate of VVC implants was 86.3%, with aseptic revisions at 84.5% and septic revisions at 88.3%, based on a median follow-up of 2.9 years. The 2-year survival rates were 92.5% overall, 88.1% for aseptic revisions, and 97.4% for septic revisions. The re-revision rate was 13.7% (22 VVC implants), primarily due to infections (86.4%).
Conclusions: VVC implants demonstrated a high 2-year survival rate of 92.5% in revision TKA at a large Asian medical institution. The most common indications for VVC implant use in revisions were infection and aseptic loosening, with infection being the leading cause of subsequent re-revisions.
Metrics
References
Lachiewicz PF, Soileau ES. Results of a second-generation constrained condylar prosthesis in primary total knee arthroplasty. J Arthroplasty 2011;26:1228-31. DOI: https://doi.org/10.1016/j.arth.2011.05.010
Mancino F, Falez F, Mocini F, et al. Is varus-valgus constraint a reliable option in complex primary total knee arthroplasty? A systematic review. J Orthop 2021;24:201-11. DOI: https://doi.org/10.1016/j.jor.2021.02.036
Nakano N, Matsumoto T, Muratsu H, et al. Revision total knee arthroplasty using the modern constrained condylar knee prosthesis. Acta Ortop Bras 2016;24:304-8. DOI: https://doi.org/10.1590/1413-785220162406146213
Hartford JM, Goodman SB, Schurman DJ, et al. Complex primary and revision total knee arthroplasty using the condylar constrained prosthesis: an average 5-year follow-up. J Arthroplasty 1998;13:380-7. DOI: https://doi.org/10.1016/S0883-5403(98)90002-X
Lachiewicz PF, Soileau ES. Ten-year survival and clinical results of constrained components in primary total knee arthroplasty. J Arthroplasty 2006;21:803-8. DOI: https://doi.org/10.1016/j.arth.2005.09.008
Touzopoulos P, Drosos GI, Ververidis A, et al. Constrained implants in total knee replacement. Surg Technol Int 2015;26:307-16.
Siqueira MB, Jacob P, McLaughlin J, et al. The varus–valgus constrained knee implant: survivorship and outcomes. J Knee Surg 2017;30:484-92. DOI: https://doi.org/10.1055/s-0036-1593361
Sabatini L, Risitano S, Rissolio L, et al. Condylar constrained system in primary total knee replacement: our experience and literature review. Ann Transl Med 2017;5:135. DOI: https://doi.org/10.21037/atm.2017.03.29
Theil C, Schwarze J, Gosheger G, et al. Good to excellent long-term survival of a single-design condylar constrained knee arthroplasty for primary and revision surgery. Knee Surg Sports Traumatol Arthrosc 2022;30:3184-90. DOI: https://doi.org/10.1007/s00167-021-06636-2
Chandran P, Patel K, Kumar V, et al. A prospective study of revision total knee replacements at a mean follow up of 11 years. Orthop Proc 2012;94-B:82.
Hovinga KR, Lerner AL. Anatomic variations between Japanese and Caucasian populations in the healthy young adult knee joint. J Orthop Res 2009;27:1191-6. DOI: https://doi.org/10.1002/jor.20858
Ha CW, Park YB, Song YS, et al. Increased range of motion is important for functional outcome and satisfaction after total knee arthroplasty in Asian patients. J Arthroplasty 2016;31:1199-203. DOI: https://doi.org/10.1016/j.arth.2015.12.018
Rosenberg AG, Verner JJ, Galante JO. Clinical results of total knee revision using the Total Condylar III prosthesis. Clin Orthop Relat Res 1991;273:83-90. DOI: https://doi.org/10.1097/00003086-199112000-00012
Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect 1999;48:167-75.
Hernandez NM, Hinton ZW, Wu CJ, et al. Varus-Valgus constrained implants in revision total knee arthroplasty: mean clinical follow-up of six years. J Arthroplasty 2021;36:S303-S7. DOI: https://doi.org/10.1016/j.arth.2020.12.017
Hegde V, Stambough JB, Levine BR, et al. Highlights of the 2022 American joint replacement registry annual report. Arthroplasty Today 2023;21:101137. DOI: https://doi.org/10.1016/j.artd.2023.101137
Quinlan ND, Werner BC, Brown TE, et al. Risk of prosthetic joint infection increases following early aseptic revision surgery of total hip and knee arthroplasty. J Arthroplasty 2020;35:3661-7. DOI: https://doi.org/10.1016/j.arth.2020.06.089
Siqueira MB, Klika AK, Higuera CA, et al. Modes of failure of total knee arthroplasty: registries and realities. J Knee Surg 2015;28:127-38. DOI: https://doi.org/10.1055/s-0034-1396014
Lee JK, Lee S, Kim D, et al. Revision total knee arthroplasty with varus-valgus constrained prosthesis versus posterior stabilized prosthesis. Knee Surg Sports Traumatol Arthrosc 2013;21:620-8. DOI: https://doi.org/10.1007/s00167-012-1998-2
Kim YH, Kim JS. Revision total knee arthroplasty with use of a constrained condylar knee prosthesis. J Bone Joint Surg Am 2009;91:1440-7. DOI: https://doi.org/10.2106/JBJS.H.00425
Hwang SC, Kong JY, Nam DC, et al. Revision total knee arthroplasty with a cemented posterior stabilized, condylar constrained or fully constrained prosthesis: a minimum 2-year follow-up analysis. Clin Orthop Surg 2010;2:112-20. DOI: https://doi.org/10.4055/cios.2010.2.2.112
Hossain F, Patel S, Haddad FS. Midterm assessment of causes and results of revision total knee arthroplasty. Clin Orthop Relat Res 2010;468:1221-8. DOI: https://doi.org/10.1007/s11999-009-1204-0
Suarez J, Griffin W, Springer B, et al. Why do revision knee arthroplasties fail?. J Arthroplasty 2008;23:99-103. DOI: https://doi.org/10.1016/j.arth.2008.04.020
Mortazavi SJ, Molligan J, Austin MS, et al. Failure following revision total knee arthroplasty: infection is the major cause. Int Orthop 2010;35:1157-64. DOI: https://doi.org/10.1007/s00264-010-1134-1
Anis HK, Sodhi N, Klika AK, et al. Is operative time a predictor for post-operative infection in primary total knee arthroplasty?. J Arthroplasty 2019;34:S331-S6. DOI: https://doi.org/10.1016/j.arth.2018.11.022
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.