Effectiveness of the Capture the Fracture Program for Patients with Hip Fractures at Phrae Hospital: A 2-Year Follow-up After Surgery
DOI:
https://doi.org/10.56929/jseaortho-2024-0224Keywords:
the CTF program, hip fracture patients, recurrent fractures, mortality rate, Multidisciplinary teamsAbstract
Purpose: To determine the effectiveness of the Capture the Fracture (CTF) program in preventing refractures, improving Barthel index scores for activities of daily living (ADL), and reducing mortality rates in patients with hip fractures.
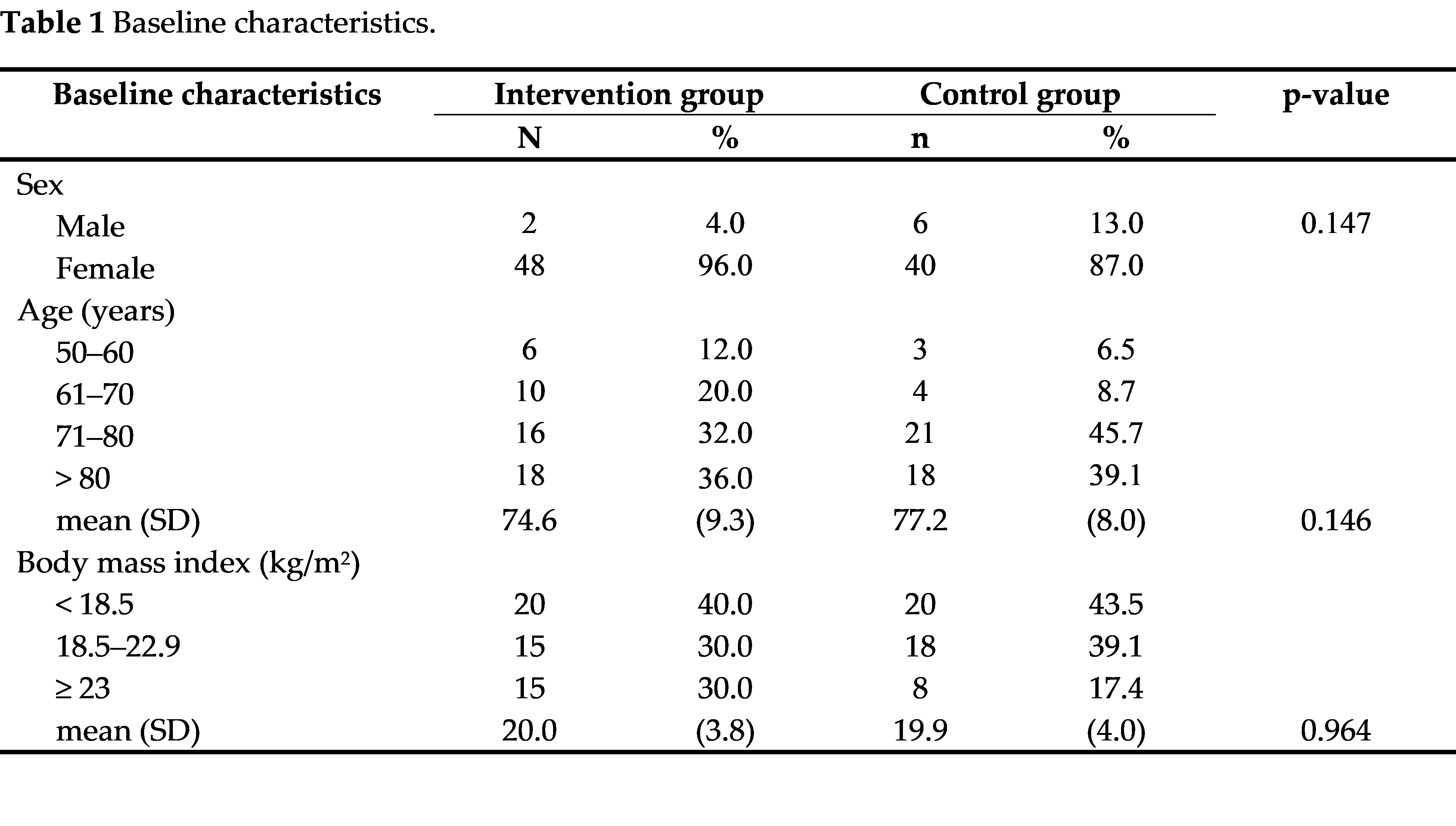
Methods: This study enrolled patients with fragile hip fractures aged ≥50 years who underwent hip fracture surgery. The participants were classified into the intervention and control groups, each consisting of 46 patients. The intervention group underwent the CTF program with a multifactorial approach, whereas the control group received routine care. Participants were followed up 1 and 2 years postoperatively to assess outcomes, including the Timed Up and Go test, balance test, Barthel index scores for ADL, fall risk assessment, refracture, and mortality rate.
Results: In the intervention group, no recurrent fractures occurred within 1 year, compared to 6.5% in the control group (p=0.106). At the 2-year postoperative follow-up, 4.9% of the intervention group experienced recurrent fractures, whereas the control group had no fractures (p=0.508). The 2-year postoperative mortality rate was 18.0% and 37.0% in the intervention and control groups, respectively (p=0.042).
Conclusions: Multidisciplinary teams should implement the CTF program using a multifactorial approach to physical rehabilitation in patients with hip fractures. This program improved participants' quality of life and reduced the mortality rate 2 years postoperatively.
Metrics
References
Wongtriratanachai P, Luevitoonvechkij S, Songpatanasilp T, et al. Increasing incidence of hip fracture in Chiang Mai, Thailand. J Clin Densitom 2013;16:347-52. DOI: https://doi.org/10.1016/j.jocd.2012.07.002
Mithal A, Ebeling P. The Asia-Pacific regional audit: epidemiology, costs and burden of osteoporosis in 2013. Switzerland: International osteoporosis foundation; 2013. DOI: https://doi.org/10.4103/2230-8210.137485
Cooper C, Atkinson EJ, O’Fallon WM, et al. Incidence of clinically diagnosed vertebral fractures: A population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res 1992;7:221-27. DOI: https://doi.org/10.1002/jbmr.5650070214
Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med 1997;103(2A):12S-17S; discussion 17S-19S. DOI: https://doi.org/10.1016/S0002-9343(97)90022-X
Autier P, Haentjens P, Bentin J, et al. Costs induced by hip fractures: a prospective controlled study in Belgium. Belgian Hip Fracture Study Group. Osteoporos Int 2000;11:373-80. DOI: https://doi.org/10.1007/s001980070102
Cree M, Soskolne CL, Belseck E, et al. Mortality and institutionalization following hip fracture. J Am Geriatr Soc 2000;48:283-88. DOI: https://doi.org/10.1111/j.1532-5415.2000.tb02647.x
Kiebzak GM, Beinart GA, Perser K, et al. Undertreatment of osteoporosis in men with hip fracture. Arch Intern Med 2002;162:2217-22. DOI: https://doi.org/10.1001/archinte.162.19.2217
Harvey NC, McCloskey EV. Gaps and solutions in bone health: a global framework for improvement. Switzerland: International osteoporosis foundation; 2016.
Harvey NCW, McCloskey EV, Mitchell PJ, et al. Mind the (treatment) cap a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int 2017;28:1507-29. DOI: https://doi.org/10.1007/s00198-016-3894-y
Garvan institute. Fracture risk calculator. 2017. Available from: http://garvan.org.au/promotions/bone-fracture-risk/calculator/. Accessed August 9, 2017.
Osnes EK, Lofthus CM, Meyer HE, et al. Consequences of hip fracture on activities of daily life and residential needs. Osteoporos Int 2004;15:567-74. DOI: https://doi.org/10.1007/s00198-003-1583-0
Gittoes N, McLellan AR, Cooper A, et al. Effective secondary prevention of fragility fractures: clinical standards for fracture liaison service. Camerton: National Osteoporosis Society; 2015.
International Osteoporosis Foundation. Capture the fracture: a global campaign to break the fragility fracture cycle. Available from: http://www.worldosteoporosisday.org/. Accessed December 17, 2012.
International Osteoporosis Foundation. Capture the fracture: break the worldwide fragility fracture cycle. Available from: http://www.osteofound.org/capture-fracture. Accessed November 1, 2012.
Srawooth P. Promotion of active aging and quality of life in old age and preparation for a complete aged society in Thailand. In: Jirakorn Y. TDRI Quarterly Review. Thailand Development Research Institute 2023;38:3-13.
Cuevas-Trisan R. Balance problems and fall risks in the elderly. Phys Med Rehabil Clin N Am 2017;28:727-37. DOI: https://doi.org/10.1016/j.pmr.2017.06.006
Prasit W, Yodpetch T, Prathoom D. Health of the Thai elderly and urban society. J Gerontol Geriatr Med 2010;11:37-41.
World Health Organization. The Heidelberg guidelines for promoting physical activity among older persons. Guidelines series for healthy aging-1; 1996.
Janz N, Champion V, Strecher V. The health belief model. In: Glanz K, Rimer BK, Lewis FM, eds. Health behavior and health education: Theory, research, and practice. 3rd ed. San Francisco, CA: Jossey-Bass; 2002. p.45-66.
Walters S, Chan S, Goh L, et al. The prevalence of frailty in patients admitted to hospital with vertebral fragility fractures. Curr Rheumatol Rev 2016;12:244-7. DOI: https://doi.org/10.2174/1573397112666160619190744
Aw D, Sahota O. Orthogeriatrics moving forward. Age Ageing 2014;43:301-5. DOI: https://doi.org/10.1093/ageing/afu011
Ensrud KE, Thompson DE, Cauley JA, et al. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture Intervention Trial Research Group. J Am Geriatr Soc 2000;48:241-9. DOI: https://doi.org/10.1111/j.1532-5415.2000.tb02641.x
Pietri M, Lucarini S. The orthopaedic treatment of fragility fractures. Clin Cases Miner Bone Metab 2007;4:108-16.
Barton DW, Piple AS, Smith CT, et al. The clinical impact of fracture liaison services: A systematic review. Geriatr Orthop Surg Rehabil 2021;12:2151459320979978. DOI: https://doi.org/10.1177/2151459320979978
Guirguis-Blake JM, Michael YL, Perdue LA, et al. Interventions to prevent falls in older adults: updated evidence report and systematic review for the US preventive services task force. JAMA 2018;319:1705-16. DOI: https://doi.org/10.1001/jama.2017.21962
Dawson-Hughes B, Mithal A, Bonjour J-P, et al. IOF position statement: vitamin D recommendations for older adults. Osteoporos Int 2010;21:1151-54. DOI: https://doi.org/10.1007/s00198-010-1285-3
Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;9:CD007146. DOI: https://doi.org/10.1002/14651858.ED000053
Bangkok hospital. Nutrition Therapy for Patients After TKR. Available from: http://www.Bangkok-hospital.com/th/nutrition-therapy-for-patients-after-tkr. Accessed June 1, 2023.
Phatthira W, Yodpiti T, Pratumtip D, et al. The Effectiveness of Phrae FLS for preventing recurrence hip fractures in hip fracture patients, Phrae Hospital. Journal of the Phrae Hospital. 2022;30:112-26.
Huntjens KM, van Geel TA, van den Bergh JP, et al. Fracture liaison service: impact on subsequent nonvertebral fracture incidence and mortality. J Bone Joint Surg Am 2014;96:e29. DOI: https://doi.org/10.2106/JBJS.L.00223
National osteoporosis society. Effective secondary prevention of fragility fractures: Clinical standards for Fracture Liaison Services. 2014. Available from: https://nos.org.uk/media/1776/clinical-standards-report.pdf. Accessed August 22, 2016.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.