Metastatic Bone Disease: A Clinical Approach
DOI:
https://doi.org/10.56929/jseaortho-2025-0226Keywords:
Clinical approach, metastases, bone, surgical guidelineAbstract
Background: Advances in oncological management have contributed to longer survival of patients, even in the presence of metastases. Consequently, more patients would be expected to present with symptomatic bony metastases. The major objectives of orthopaedic surgical interventions in bone metastases include stabilization of impending or actual pathological fractures, restoration of mobility and gait, with resultant reduction in the overall morbidity during the survival period of the cancer patient.
Purpose: This review was aimed at producing a synoptic material for ease of reference by students, trainees and young surgeons who come into contact with patients suffering from metastatic bone lesions.
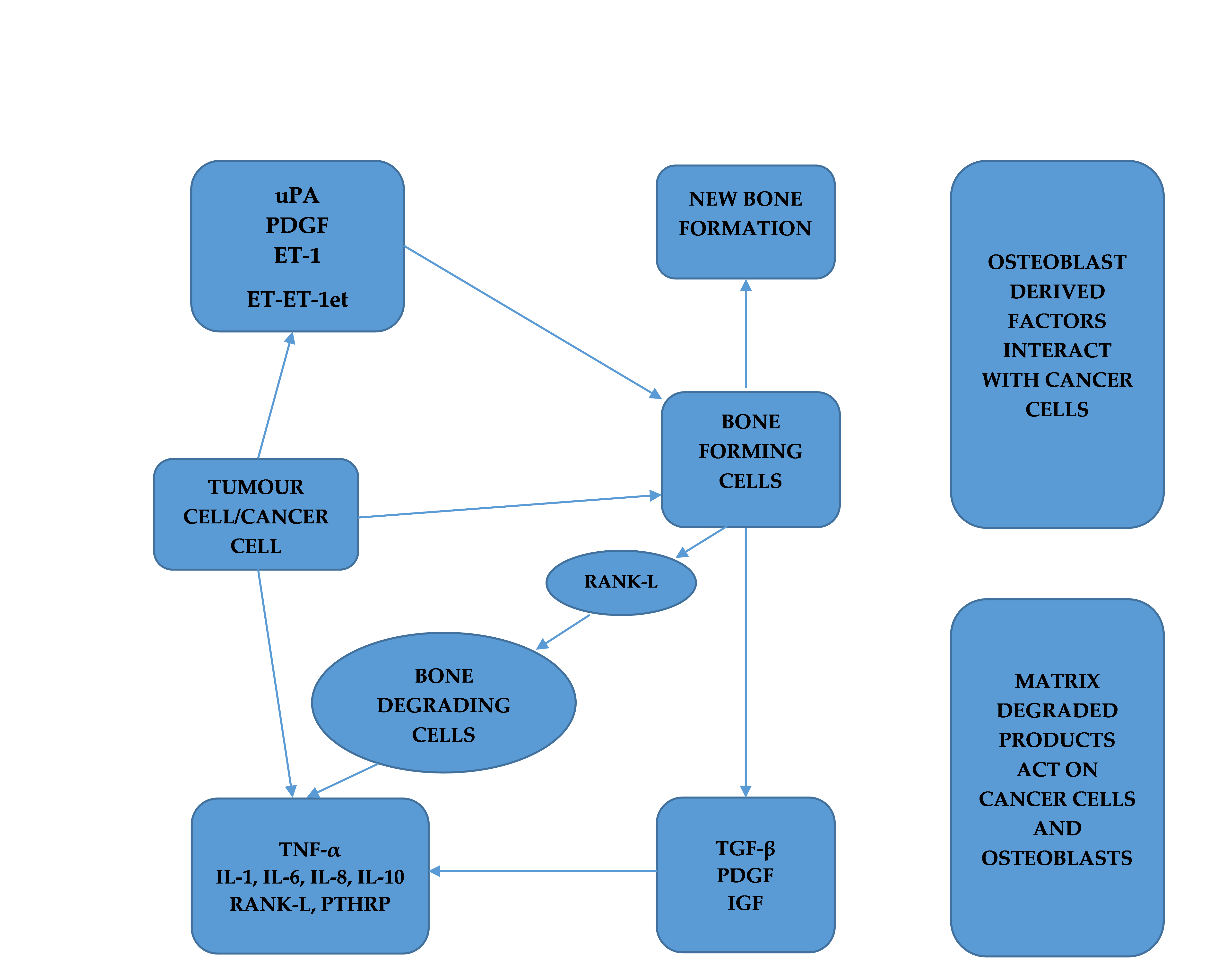
Methods: A review of the literature on the subject of metastatic bone diseases was done. Information on epidemiology, pathophysiology and mechanisms of bone metastases, clinical problems and concept of skeletal related events (SREs), differential diagnoses, diagnostic approach, general principles and options of treatment, and prognosis was extracted and presented.
Conclusions: Metastatic lesions are the most common malignant tumours that affect the skeleton, and these malignant deposits in bones increase overall morbidity in cancer patients. Appendicular skeleton offers a large surface area for deposition of tumour cells from primary sites, including the breast, prostate, lung, kidney and thyroid, with the highest incidence coming from breast and prostate. The osseous lesions of primary malignant diseases predispose to pain, mechanical instability and fractures in the affected parts. These factors contribute to the overall morbidity and reduced survival in cancer patients.
Metrics
References
Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 2006;12:6243s-9s. DOI: https://doi.org/10.1158/1078-0432.CCR-06-0931
Utzschneider S, Wicherek E, Weber P, et al. Surgical treatment of bone metastases in patients with lung cancer. Int Orthop 2010;35:731-6. DOI: https://doi.org/10.1007/s00264-010-1074-9
Teixeira LEM, Miranda RH, Ghedini DF, et al. Early complications in the Orthopaedic treatment of bone metastases. Rev Bras Ortop 2009;44:519-23. DOI: https://doi.org/10.1016/S2255-4971(15)30151-8
Dim EM, Yau CHR, Ho WYK, et al. Profile of surgically-treated metastatic extremity bone tumours at a University Hospital in Hong Kong. J Orthop Trauma Rehabil 2018;24:1-8. DOI: https://doi.org/10.1016/j.jotr.2017.03.002
Riccio AI, Wodajo FM, Malawer M. Metastatic carcinoma of the long bones. Am Fam Physician 2007;76:1489-94.
Guzik G. Results of the treatment of bone metastases with modular prosthetic replacement - analysis of 67 patients. J Orthop Surg Res 2016; 11:20. DOI: https://doi.org/10.1186/s13018-016-0353-6
Schulman KL, Kohles J. Economic burden of metastatic bone disease in the U.S. Cancer 2007; 109:2334-42. DOI: https://doi.org/10.1002/cncr.22678
Yin JJ, Pollock CB, Kelly K. Mechanisms of cancer metastasis to the bone. Cell Res 2005;15:57-62. DOI: https://doi.org/10.1038/sj.cr.7290266
Jeremic B, Watanabe N. Criteria for palliation of bone metastases - clinical applications. Vienna : International Atomic Energy Agency. 2007. Available from: https://www-pub.iaea.org/MTCD/publications/PDF/te_1549_web.pdf. Accessed April, 2007.
Mundy GR, Yoneda T. Facilitation and suppression of bone metastasis. Clin Orthop Relat Res 1995;(312):34-44.
Guise TA, Yin JJ, Taylor SD, et al. Evidence for a causal role of parathyroid hormone-related protein in the pathogenesis of human breast cancer-mediated osteolysis. J Clin Invest 1996;98: 1544-9. DOI: https://doi.org/10.1172/JCI118947
Ban J, Fock V, Aryee DNT, et al. Mechanisms, diagnosis and treatment of bone metastases. Cells 2021;10:2944. DOI: https://doi.org/10.3390/cells10112944
Obenauf AC, Massagué J. Surviving at a distance: organ specific metastasis. Trends Cancer 2015;1:76-91. DOI: https://doi.org/10.1016/j.trecan.2015.07.009
Zhang X. Interactions between cancer cells and bone microenvironment promote bone metastasis in prostate cancer. Cancer Commun (Lond) 2019;39:76. DOI: https://doi.org/10.1186/s40880-019-0425-1
Valastyan S, Weinberg RA. Tumor metastasis: molecular insights and evolving paradigms. Cell 2011; 147: 275-92. DOI: https://doi.org/10.1016/j.cell.2011.09.024
Fidler IJ. Metastasis: quantitative analysis of distribution and fate of tumor emboli labeled with 125 I-5-iodo-2'-deoxyuridine. J Natl Cancer Inst 1970;45:773-82.
Yu M, Bardia A, Wittner BS, et al., Circulating breast tumor cells exhibit dynamic changes in epithelial and mesenchymal composition. Science 2013;339:580-4. DOI: https://doi.org/10.1126/science.1228522
Bussard KM, Gay CV, Mastro AM. The bone microenvironment in metastasis; what is special about bone?. Cancer Metastasis Rev 2008;27:41-55. DOI: https://doi.org/10.1007/s10555-007-9109-4
Dim EM, Nottidge TE, Miriam DU, et al. Adenocarcinoma of the colon presenting as bone metastases of unknown primary. J of Biomed & Clin Sci 2020;5:49-55.
Rolfo C, Raez LE, Russo A, et al. Molecular target therapy for bone metastasis: Starting a new era with denosumab, a RANKL inhibitor. Expert Opin Biol Ther 2014;14:15-26. DOI: https://doi.org/10.1517/14712598.2013.843667
Johnstone RH, Ardern DW, Bartle DR. Multifocal skeletal tuberculosis masquerading as metastatic disease. ANZ J Surg 2011;81:731-3. DOI: https://doi.org/10.1111/j.1445-2197.2011.05844.x
Hasegawa K, Murata H, Naitoh K, et al. Spinal tuberculosis: report of an atypical presentation. Clin Orthop Relat Res 2002;(403):100-3. DOI: https://doi.org/10.1097/00003086-200210000-00016
Maduakonam DE, Lee LY, Tony WS, et al. Tuberculous osteomyelitis of the proximal femur masquerading as bone secondary: A case report. J Orthop Trauma Rehabil 2020;27:1-5. DOI: https://doi.org/10.1177/2210491720907492
Su M, Fan Q, Fan C, et al. Lung sequestration and Potts’ disease masquerading as primary lung cancer with bone metastases on FDG PET/CT. Clin Nucl Med 2009;34:236-8. DOI: https://doi.org/10.1097/RLU.0b013e31819a20a1
Mirels H. Metastatic disease in long bones: A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 1989;249:256-64 DOI: https://doi.org/10.1097/00003086-198912000-00027
Jawad MU, Scully SP. In brief: classifications in brief: Mirels' classification: metastatic disease in long bones and impending pathologic fracture. Clin Orthop Relat Res 2010;468:2825-7. DOI: https://doi.org/10.1007/s11999-010-1326-4
Siddique I, Stirling AJ. Focus on the surgical management of spinal cord compression. J Bone Joint Surg Br [serial online]. 2010; 1-5. Available from: http://www. http://www.boneandjoint.org.uk/content/focus/surgical-management-metastatic-spinal-cord-compression.
Li AA, Cao ZY, Liu JM, et al. The risk factors for bone metastases in patients with colorectal cancer. Medicine (Baltimore) 2018;97:e12694. DOI: https://doi.org/10.1097/MD.0000000000012694
Hung HY, Chen JS, YuhYeh C, et al. Preoperative alkaline phosphatase elevation was associated with poor survival in colorectal cancer patients. Int J Colorectal Dis 2017;32:1775-8. DOI: https://doi.org/10.1007/s00384-017-2907-4
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.