Early Hip Dislocation Rate in a Consecutive Series of 1093 Primary Total Hip Arthroplasties Using Imageless Navigation
DOI:
https://doi.org/10.56929/jseaortho-2024-0230Keywords:
Primary, Total hip arthroplasty, Dislocation, Imageless computer navigationAbstract
Purpose: Postoperative hip dislocation remains a major complication in total hip arthroplasty. Various studies have demonstrated that several factors influence dislocation. While computer-assisted navigation has been proposed to enhance component alignment, its impact on dislocation rates remains unclear. This study aimed to investigate the early dislocation incidence and associated risk factors in primary total hip arthroplasty (THA) using imageless navigation.
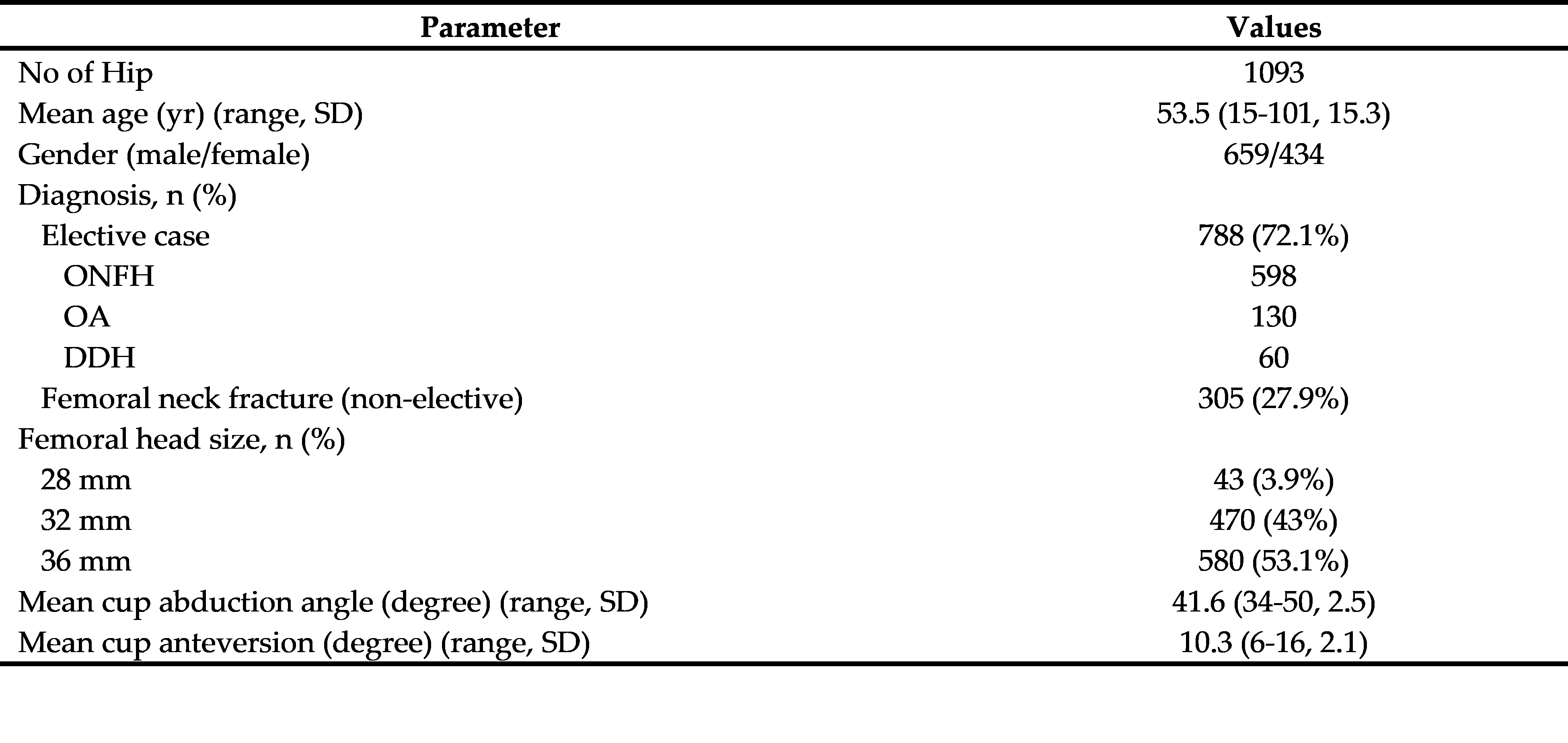
Methods: A retrospective review of patients undergoing imageless-navigated THA between February 2013 and December 2022 was conducted. Inclusion criteria comprised primary THA with a minimum 6-month follow-up. Statistical analysis included univariate regression to identify dislocation risk factors.
Results: A total of 1093 THAs were analyzed. Dislocation occurred in 16 cases (1.5%), six in elective procedures (0.76%), and 10 in femoral neck fracture (FNF) (3.28%). The univariate regression analysis revealed that FNF emerged as a significant risk factor (OR = 4.418, P = 0.004), while age, gender, femoral head size, and save zone cup placement of Lewinnek did not significantly affect dislocation rates.
Conclusions: Navigation use showed a reduced rate of early dislocation. FNF is a factor associated with postoperative hip dislocation in primary THA.
Metrics
References
Gwam CU, Mistry JB, Mohamed NS, et al. Current epidemiology of revision total hip arthroplasty in the United States: National inpatient sample 2009 to 2013. J Arthroplasty 2017;32:2088-92. DOI: https://doi.org/10.1016/j.arth.2017.02.046
Abdel MP, Cross MB, Yasen AT, et al. The functional and financial impact of isolated and recurrent dislocation after total hip arthroplasty. Bone Joint J 2015;97-B:1046-9. DOI: https://doi.org/10.1302/0301-620X.97B8.34952
Sanchez-Sotelo J, Haidukewych GJ, Boberg CJ. Hospital cost of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am 2006;88:290-4. DOI: https://doi.org/10.2106/JBJS.D.02799
Coventry MB, Beckenbaugh RD, Nolan DR, et al. 2,012 total hip arthroplasties. A study of postoperative course and early complications. J Bone Joint Surg Am 1974;56:273-84. DOI: https://doi.org/10.2106/00004623-197456020-00005
Nolan DR, Fitzgerald RH Jr, Beckenbaugh RD, et al. Complications of total hip arthroplasty treated by reoperation. J Bone Joint Surg Am 1975;57:977-81. DOI: https://doi.org/10.2106/00004623-197557070-00017
Fukumori N, Sonohata M, Kitajima M, et al. Reduction of postoperative pain by addition of intravenous acetaminophen after total hip arthroplasty: A retrospective cohort study. Acta Med Okayama 2019;73:7-14.
Leong JW, Cook MJ, O'Neill TW, et al. Is the use of antibiotic-loaded bone cement associated with a lower risk of revision after primary total hip arthroplasty?. Bone Joint J 2020;102-B:997-1002. DOI: https://doi.org/10.1302/0301-620X.102B8.BJJ-2020-0120.R1
Ding Y, Feng D, Liu Y, et al. The prevalence and risk factors of dislocation after primary total hip arthroplasty. Acta Orthop Belg 2022;88:467-74. DOI: https://doi.org/10.52628/88.3.9760
Kunutsor SK, Barrett MC, Beswick AD, et al. Risk factors for dislocation after primary total hip replacement: a systematic review and meta-analysis of 125 studies involving approximately five million hip replacements. Lancet Rheumatol 2019;1:e111-21. DOI: https://doi.org/10.1016/S2665-9913(19)30045-1
Berry DJ, von Knoch M, Schleck CD, et al. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am 2005;87:2456-63. DOI: https://doi.org/10.2106/00004623-200511000-00012
Buckland AJ, Puvanesarajah V, Vigdorchik J, et al. Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Joint J 2017;99-B:585-91. DOI: https://doi.org/10.1302/0301-620X.99B5.BJJ-2016-0657.R1
Wera GD, Ting NT, Moric M, et al. Classification and management of the unstable total hip arthroplasty. J Arthroplasty 2012;27:710-5. DOI: https://doi.org/10.1016/j.arth.2011.09.010
Suksathien Y, Suksathien R, Chaiwirattana P. Acetabular cup placement in navigated and non-navigated total hip arthroplasty (THA): results of two consecutive series using a cementless short stem. J Med Assoc Thai 2014;97:629-34.
Mainard D. Navigated and nonnavigated total hip arthroplasty: results of two consecutive series using a cementless straight hip stem. Orthopedics 2008;31(10 Suppl 1):orthosupersite.com/view.asp?rID=35528.
Kalteis T, Handel M, Herold T, et al. Greater accuracy in positioning of the acetabular cup by using an image-free navigation system. Int Orthop 2005;29:272-6. DOI: https://doi.org/10.1007/s00264-005-0671-5
Kalteis T, Handel M, Bäthis H, et al. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation?. J Bone Joint Surg Br 2006;88:163-7. DOI: https://doi.org/10.1302/0301-620X.88B2.17163
Lass R, Olischar B, Kubista B, et al. Total hip arthroplasty using imageless computer-assisted navigation-2-year follow-up of a prospective randomized study. J Clin Med 2020;9:1620. DOI: https://doi.org/10.3390/jcm9061620
Leenders T, Vandevelde D, Mahieu G, et al. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg 2002;7:99-106. DOI: https://doi.org/10.1002/igs.10033
Parratte S, Argenson JN. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. A prospective, randomized, controlled study. J Bone Joint Surg Am 2007;89:494-9. DOI: https://doi.org/10.2106/JBJS.F.00529
Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 1978;60:217-20. DOI: https://doi.org/10.2106/00004623-197860020-00014
Suksathien Y, Suksathien R, Chaiwirattana P. Accuracy of acetabular cup placement in navigated THA with modified registration technique in semilateral decubitus position. J Med Assoc Thai 2014;97:1089-95.
Agarwal S, Eckhard L, Walter WL, et al. The use of computer navigation in total hip arthroplasty is associated with a reduced rate of revision for dislocation: A study of 6,912 navigated THA procedures from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am 2021;103:1900-5. DOI: https://doi.org/10.2106/JBJS.20.00950
Liaw CK, Hou SM, Yang RS, et al. A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs. Clin Orthop Relat Res 2006;451:134-9. DOI: https://doi.org/10.1097/01.blo.0000223988.41776.fa
Park YS, Shin WC, Lee SM, et al. The best method for evaluating anteversion of the acetabular component after total hip arthroplasty on plain radiographs. J Orthop Surg Res 2018;13:66. DOI: https://doi.org/10.1186/s13018-018-0767-4
Bohl DD, Nolte MT, Ong K, et al. Computer-assisted navigation is associated with reductions in the rates of dislocation and acetabular component revision following primary total hip arthroplasty. J Bone Joint Surg Am 2019;101:250-6. DOI: https://doi.org/10.2106/JBJS.18.00108
Gausden EB, Parhar HS, Popper JE, et al. Risk factors for early dislocation following primary elective total hip arthroplasty. J Arthroplasty 2018;33:1567-71.e2. DOI: https://doi.org/10.1016/j.arth.2017.12.034
Pangaud C, Pioger C, Pauly V, et al. Total hip arthroplasty reduces the risk of dislocation after femoral neck fracture. Orthop Traumatol Surg Res 2023;109:103575. DOI: https://doi.org/10.1016/j.otsr.2023.103575
Kelley SS, Lachiewicz PF, Hickman JM, et al. Relationship of femoral head and acetabular size to the prevalence of dislocation. Clin Orthop Relat Res. 1998;(355):163-70. DOI: https://doi.org/10.1097/00003086-199810000-00017
Singh SP, Bhalodiya HP. Head size and dislocation rate in primary total hip arthroplasty. Indian J Orthop 2013;47:443-8. DOI: https://doi.org/10.4103/0019-5413.118198
Hedlundh U, Ahnfelt L, Hybbinette CH, et al. Dislocations and the femoral head size in primary total hip arthroplasty. Clin Orthop Relat Res 1996;(333):226-33. DOI: https://doi.org/10.1097/00003086-199612000-00024
Abdel MP, von Roth P, Jennings MT, et al. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res 2016;474:386-91. DOI: https://doi.org/10.1007/s11999-015-4432-5
Bargar WL, Bauer A, Börner M. Primary and revision total hip replacement using the Robodoc system. Clin Orthop Relat Res 1998;(354):82-91. DOI: https://doi.org/10.1097/00003086-199809000-00011
Honl M, Dierk O, Gauck C, et al. Comparison of robotic-assisted and manual implantation of a primary total hip replacement. A prospective study. J Bone Joint Surg Am 2003;85:1470-8. DOI: https://doi.org/10.2106/00004623-200308000-00007
Kamara E, Robinson J, Bas MA, et al. Adoption of robotic vs fluoroscopic guidance in total hip arthroplasty: Is acetabular positioning improved in the learning curve?. J Arthroplasty 2017;32:125-30. DOI: https://doi.org/10.1016/j.arth.2016.06.039
Nakamura N, Sugano N, Nishii T, et al. Robot-assisted primary cementless total hip arthroplasty using surface registration techniques: a short-term clinical report. Int J Comput Assist Radiol Surg 2009;4:157-62. DOI: https://doi.org/10.1007/s11548-009-0286-1
Nakamura N, Sugano N, Nishii T, et al. A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res 2010;468:1072-81. DOI: https://doi.org/10.1007/s11999-009-1158-2
Siebel T, Käfer W. Klinisches Outcome nach Roboter-assistierter versus konventionell implantierter Hüftendoprothetik: Prospektive, kontrollierte Untersuchung von 71 Patienten [Clinical outcome following robotic assisted versus conventional total hip arthroplasty: a controlled and prospective study of seventy-one patients]. Z Orthop Ihre Grenzgeb 2005;143:391-8. DOI: https://doi.org/10.1055/s-2005-836776
Lewis DP, Wæver D, Thorninger R, et al. Hemiarthroplasty vs total hip arthroplasty for the management of displaced neck of femur fractures: A systematic review and meta-analysis. J Arthroplasty 2019;34:1837-43.e2. DOI: https://doi.org/10.1016/j.arth.2019.03.070
Byström S, Espehaug B, Furnes O, et al. Femoral head size is a risk factor for total hip luxation: a study of 42,987 primary hip arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop Scand 2003;74:514-24. DOI: https://doi.org/10.1080/00016470310017893
Inacio MC, Ake CF, Paxton EW, et al. Sex and risk of hip implant failure: assessing total hip arthroplasty outcomes in the United States. JAMA Intern Med 2013;173:435-41. DOI: https://doi.org/10.1001/jamainternmed.2013.3271
Jørgensen CC, Kjaersgaard-Andersen P, Solgaard S, et al. Hip dislocations after 2,734 elective unilateral fast-track total hip arthroplasties: incidence, circumstances and predisposing factors. Arch Orthop Trauma Surg 2014;134:1615-22. DOI: https://doi.org/10.1007/s00402-014-2051-3
Fessy MH, Putman S, Viste A, et al. What are the risk factors for dislocation in primary total hip arthroplasty? A multicenter case-control study of 128 unstable and 438 stable hips. Orthop Traumatol Surg Res 2017;103:663-8. DOI: https://doi.org/10.1016/j.otsr.2017.05.014
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.