Combined Vertebral Fracture Assessment and FRAX Tool Thailand With or Without Bone Mineral Density for Diagnosis of Osteoporosis in Elderly
DOI:
https://doi.org/10.56929/jseaortho-2025-0248Keywords:
osteoporosis diagnosis, vertebral fracture assessment, FRAX, Bone mineral densityAbstract
Purpose: To evaluate the reliability of using vertebral fracture assessment by radiography (VFA) in combination with FRAX tool Thailand to diagnose osteoporosis in elderly patients, without the need for bone mineral density (BMD) measurement.
Methods: All elderly individuals who fulfill the criteria for osteoporosis assessment according to the 2021 CPG for osteoporosis care by the Thailand osteoporosis foundation were assessed BMD, VFA, and FRAX tool Thailand with and without BMD. Fracture risk was first evaluated using only FRAX without BMD and the presence of asymptomatic vertebral fractures (AVF). The second assessment used FRAX with BMD, the results of BMD measurements, and the presence of AVF. The results of these two assessments were compared to evaluate the reliability of the osteoporotic diagnosis.
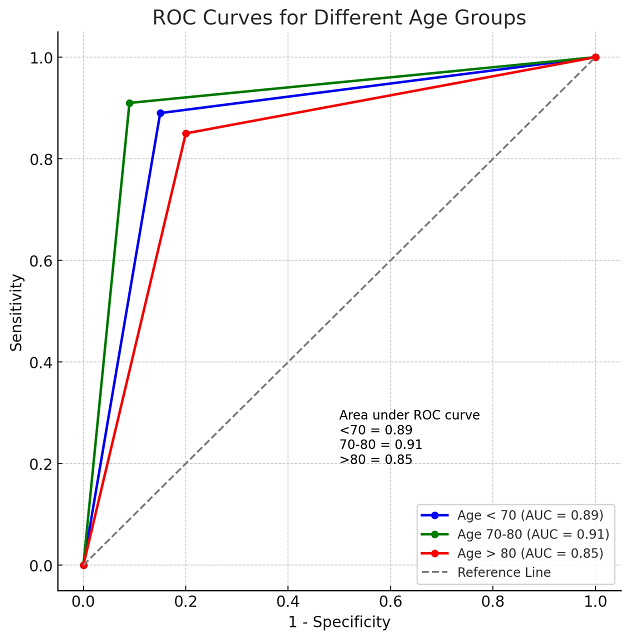
Results: The prevalence of osteoporosis in the study was found to be 67% (95% CI: 60%–72.9%). The test exhibited high sensitivity (90.6%, 95% CI: 84.5%–94.9%) and specificity (92.9%, 95% CI: 84.1%–97.6%), indicating its strong ability to accurately identify both individuals with and without osteoporosis. The Receiver Operating Characteristic (ROC) area of 0.918 (95% CI: 0.879–0.956). For subgroup analysis, in males (n=44), the test demonstrated excellent performance with a sensitivity of 95.2%, specificity of 100%, and a sensitivity of 89.8% and specificity of 89.4% in females (n=165). In the age-based subgroup analysis, the results in those aged >80 years (n=35) had highest sensitivity at 96.8% but lower specificity at 75.0%. For participants aged 70-80 years (n=84), sensitivity was 94.7%, and specificity was 88.9%. The youngest group, aged <70 years (n=90), had the lowest sensitivity of 82.4% but a high specificity of 97.4%. The ROC area ranged from 0.85 in those >80 years, 0.89 in those <70 years, and 0.91 in the aged 70-80 years group.
Conclusions: The combined use of VFA and FRAX without BMD offers a simple, highly effective method for diagnosing osteoporosis in elderly patients, especially in all men and women aged 70-80 years at minimal cost.
Metrics
References
Department of Medical Services, Ministry of Public Health. Clinical practice guidelines for osteoporosis. In: Wattana P, editor. Bangkok: The Agricultural Co-operative Federation of Thailand, LTD; 2005.
Sakolsattayathorn P. Campaign to reduce recurrent hip fractures in the elderly on World Osteoporosis Day. Ministry of Public Health. Available from: https://www.hfocus.org/content/2017/10/14772. Accessed October 22, 2017.
Limthongkul M. Fracture in elderly. Ramathibodi Nursing Journal 2015;2:99-111.
Salari N, Ghasemi H, Mohammadi L, et al. The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg Res 2021;16:609. DOI: https://doi.org/10.1186/s13018-021-02772-0
Chariyalertsak S, Suriyawongpisal P, Thakkinstain A. Mortality after hip fractures in Thailand. Int Orthop 2001;25:294-7. DOI: https://doi.org/10.1007/s002640100270
Leslie WD, Tsang JF, Caetano PA, et al. Effectiveness of bone density measurement for predicting osteoporosis fractures in clinical practice. J Clin Endocrinol Metab 2007;92:77-81. DOI: https://doi.org/10.1210/jc.2006-1415
Ross PD, Davis JW, Epstein RS, et al. Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Ann Intern Med 1991;114:919-23. DOI: https://doi.org/10.7326/0003-4819-114-11-919
Melton LJ, Atkinson EJ, Cooper C, et al. Vertebral fractures predict subsequent fractures. Osteoporos Int 1999;10:214-21. DOI: https://doi.org/10.1007/s001980050218
Jager PL, HJA Slart R, Webber CL, et al. Combined vertebral fracture assessment and bone mineral density measurement: a patient-friendly new tool with an important impact on the Canadian Risk Fracture Classification. Can Assoc Radiol J 2010;61:194-200. DOI: https://doi.org/10.1016/j.carj.2009.12.012
Schousboe JT, Lix LM, Morin SN, et al. Vertebral fracture assessment increases use of pharmacologic therapy for fracture prevention in clinical practice. J Bone Miner Res 2019;34:2205-12. DOI: https://doi.org/10.1002/jbmr.3836
Schousboe JT, Lix LM, Morin SN, et al. Prevalent vertebral fracture on bone density lateral spine (VFA) images in routine clinical practice predict incident fractures. Bone 2019:121:72-9. DOI: https://doi.org/10.1016/j.bone.2019.01.009
Charatcharoenwitthaya N, Jaisamrarn U, Songpatanasilp T, et al. Summary of the Thai Osteoporosis Foundation (TOPF) Clinical Practice Guideline on the diagnosis and management of osteoporosis 2021. Osteoporos Sarcopenia 2023;9:45-52. DOI: https://doi.org/10.1016/j.afos.2023.06.001
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA 2001;285:785-95. DOI: https://doi.org/10.1001/jama.285.6.785
Grigoryan M, Guermazi A, Roemer FW, et al. Recognizing and reporting osteoporotic vertebral fractures. Eur Spine J 2003;12 Suppl 2:S104-12 DOI: https://doi.org/10.1007/s00586-003-0613-0
Lenchik L, Rogers LF, Delmas PD,et al. Diagnosis of osteoporotic vertebral fractures: importance of recognition and description by radiologists. AJR Am J Roentgenol 2004;183:949-58 DOI: https://doi.org/10.2214/ajr.183.4.1830949
Genant HK, Wu CY, van Kuijk C, et al. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8:1137-48 DOI: https://doi.org/10.1002/jbmr.5650080915
Dawson-Hughes B, Tosteson ANA, Melton 3rd LJ, et al. Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the USA. Osteoporos Int 2008;19:449-58 DOI: https://doi.org/10.1007/s00198-008-0559-5
Unnanuntana A, Brian G, Eve D, et al. The assessment of fracture risk. J Bone Joint Surg Am 2010;92:743-53. DOI: https://doi.org/10.2106/JBJS.I.00919
Asavamongkolkul A, Adulkasem N, Chotiyarnwong P, et al. Prevalence of osteoporosis, sarcopenia, and high falls risk in healthy community-dwelling Thai older adults: a nationwide cross-sectional study. JBMR Plus 2024;8:ziad020. DOI: https://doi.org/10.1093/jbmrpl/ziad020
Schousboe JT, Debold CR. Reliability and accuracy of vertebral fracture assessment with densitometry compared to radiography in clinical practice. Osteoporos Int 2006;17:281-9. DOI: https://doi.org/10.1007/s00198-005-2010-5
Cui L, Chen L, Xia W, et al. Vertebral fracture in postmenopausal Chinese women: a population-based study. Osteoporos Int 2017;28:2583-90. DOI: https://doi.org/10.1007/s00198-017-4085-1
Gadam RK, Schlauch K, Izuora KE. Frax prediction without BMD for assessment of osteoporotic fracture risk. Endocr Pract 2013;19:780-4. DOI: https://doi.org/10.4158/EP12416.OR
Sribenjalak D, Charoensri S, Pongchaiyakul C. An optimal intervention threshold of FRAX in postmenopausal Thai women. Arch Osteoporos 2022;17:21. DOI: https://doi.org/10.1007/s11657-022-01058-0
Johansson L, Johansson H, Axelsson KF, et al. Improved fracture risk prediction by adding VFA-identified vertebral fracture data to BMD by DXA and clinical risk factors used in FRAX. Osteoporos Int 2022;33:1725-38. DOI: https://doi.org/10.1007/s00198-022-06387-x
Kılıç Z, Alkan BM. The frequency of spontaneous vertebral fracture in geriatric patients and the relationship of vertebral fractures with age: a retrospective study. Turk J Osteoporos 2021;27:90-5. DOI: https://doi.org/10.4274/tod.galenos.2020.26576
Liao EY, Wu XP, Deng XG, et al. Age-related bone mineral density, accumulated bone loss rate and prevalence of osteoporosis at multiple skeletal sites in chinese women. Osteoporos Int 2002;13:669-76. DOI: https://doi.org/10.1007/s001980200091
Wells G, Cranney A, Peterson J, et al. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev 2008:(1):CD004523. DOI: https://doi.org/10.1002/14651858.CD004523.pub3
Wells GA, Cranney A, Peterson J, et al. Etidronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev 2008;2008:CD003376. DOI: https://doi.org/10.1002/14651858.CD003376.pub3
Wells GA, Cranney A, Peterson J, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev 2008:(1):CD001155. DOI: https://doi.org/10.1002/14651858.CD001155.pub2
Schousboe JT, Ensrud KE, Nyman JA, et al. Cost-effectiveness of vertebral fracture assessment to detect prevalent vertebral deformity and select postmenopausal women with a femoral neck T-score > -2.5 for alendronate therapy: a modeling study. JCD 2006;9:133-43. DOI: https://doi.org/10.1016/j.jocd.2005.11.004
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 The Royal College of Orthopaedic Surgeons of Thailand

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.